Borderline Personality Disorder Attachment Therapy
In clinical settings, few labels evoke as much apprehension as “Borderline Personality Disorder.”
It’s not uncommon to hear clinicians say:
“I’m not sure I could cope.”
“They’re too demanding.”
“I’m afraid I’ll be overwhelmed.”
That fear is not understandable—but is it justified?
Underneath the diagnostic criteria lies something familiar to many of us: disorganised attachment, early trauma, and profound shame.
The Attachment Wound at the Core
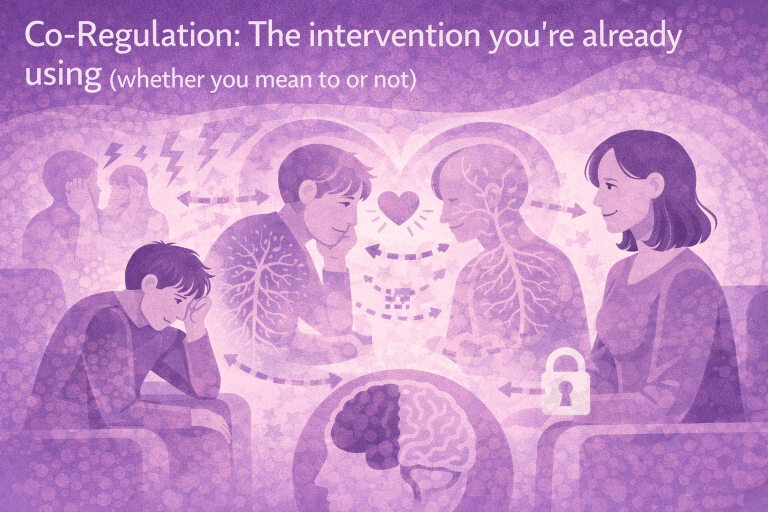
As explored by Fonagy & Bateman in their work on Mentalisation-Based Therapy (MBT), clients with BPD often struggle to mentalise—especially under relational stress. When early caregivers were frightening or inconsistent, these clients learnt to survive by splitting, projecting, and becoming hypervigilant.
Our Attachment Psychotherapeutic Counselling Diploma encourages understanding. These are powerful insights:-
“Infants whose attachments are typified by ‘fright without solution’… show early signs of disturbance.”
What often gets interpreted as manipulation is, in reality, survival behaviour rooted in a relational double-bind.
So What Helps?
Therapy doesn’t need to be about fixing. It’s about:
- Creating safety through structure, consistency, and clarity
- Offering a mentalising presence—curiosity, not certainty
- Valuing being without overdoing to
In other words, the task is to become a secure enough other when the client cannot regulate alone.
Therapists needn’t be saviours. But we do need to be grounded, present, and able to tolerate distress without jumping to rescue. As one training slide reminded us: “Compassion can tolerate distress without needing to fix it.”
A Reframe for Practitioners
Let’s say this clearly:
Clients with BPD aren’t “too much.”
They’re often people who’ve had too much to carry alone.
With proper support, supervision, and reflective practice, we can offer them a different relational experience—one that fosters regulation, self-worth, and ultimately, healing.
It’s time to shift the narrative. Let’s replace fear with understanding and clinical caution with compassionate skill.